Forward Pelvis: the Good, the Bad, and the Ugly
Opinions on what constitutes a pelvic problem abound. The term "forward pelvis" with its negative connotation, has come to be used for an assortment of pelvic / lumbar architectures, some of which, according to the Gokhale Method - are good, and some bad.
Have you been diagnosed with “forward pelvis” (aka “anterior pelvic tilt”)? If so, you may be concerned about the Gokhale Method recommendation to antevert your pelvis, thinking that this will exacerbate the problem.
Your confusion is not unique. Very few professionals, whether doctors, trainers, or wellness practitioners, differentiate between “forward pelvis / anterior pelvic tilt” and healthy pelvic anteversion. This can lead to poor recommendations like tucking your pelvis or doing crunches.

A common approach to fixing pelvic problems in modern times is the pelvic tuck and crunches, both of which carry significant risks. The Gokhale Method has different (and we believe better) solutions to various pelvic or lumbar issues that students may have.
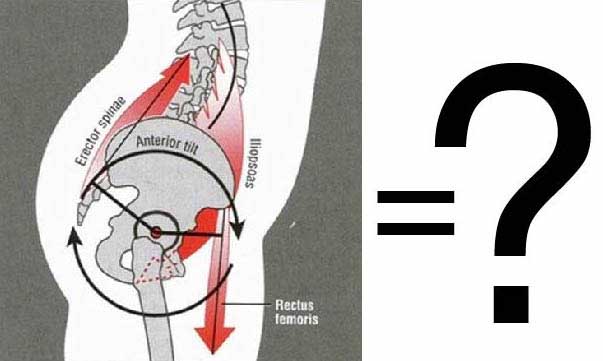
Anterior rotation of the pelvis on its own is not the problem. It’s where else you rotate and how that marks the critical difference between a happy and an unhappy spine.
“Forward pelvis” is vague terminology that is used to describe a variety of spinal architectures that share the common (and not very revealing) element that the pelvis is inclined forward relative to the ground. The term does not distinguish between curves that occur high in the lumbar spine, which are liable to cause pain and dysfunction, and the curve that happens at L5-S1 which is normal and healthy.
Healthy pelvic anteversion occurs only between the lowest of the free vertebrae in a human spine (known as L5), and the top of the sacrum (known as S1). If the L5-S1 angle is intact, it’s possible to stack the entire vertebral column with little effort.
With a "Forward pelvis”, the rotation is not necessarily isolated at L5-S1—in fact, there may be no rotation at all at that point—and usually there is rotation at one or more adjacent vertebrae.
Curvature at L5-S1 and lumbar region | Upper lumbar curvature; none at L5-S1 | Curvature solely at L5-S1 |
|
|
|
Arthur White, MD, The Posture Prescription | ©2016 Gokhale Method |
In the Gokhale Method Foundations course, students work with a teacher to find a suitably shaped wedge to support their particular L5-S1 architecture. Once students learn how to sit with an appropriately rotated pelvis, they are often surprised by how effortlessly they can now remain upright. With the pelvis properly anteverted, the rest of the spine stacks and the back muscles can actually relax.

Student Travis Dunn’s Before and After sitting pictures. Taking the Gokhale Method Foundations course helped him find a sweet spot that got rid of his longstanding back problem.
Even though this is how you sat naturally when you were quite small, it can take some coaching to release the muscles previously needed to work to hold you upright!
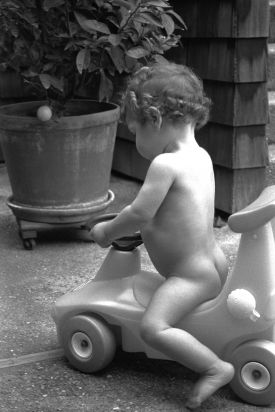
Nathan White (left), 1993, and Monisha White (right), 1996, displaying the natural and healthy pelvic anteversion shared by all young children. Notice that their pelvises tip forward in isolation from the lumbar spine.
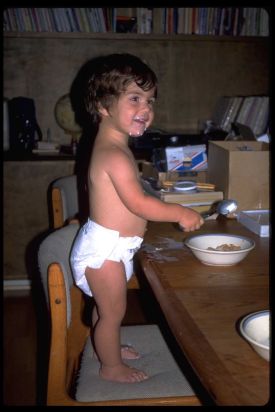
What is unhealthy about most instances of “forward pelvis”? Let take a look at the physiology of the spine. Your vertebrae are cylindrical bones and in between each vertebra is an equally cylindrical disc that functions as a shock absorber.

Your spinal discs are shock absorbers. Most spinal discs are cylindrical in shape.
The L5-S1 disc at the bottom of the stack is unique among spinal discs in being wedge-shaped, with the broad edge of the wedge toward the front of the body. If you arch the spine, each cylindrical disc is forced into a wedge shape. Likewise, if the proper anteversion is not achieved at L5-S1, and there is some degree of tucking of the pelvis, the naturally wedge-shaped L5-S1 disc gets pinched into a more cylindrical form. After years of distorting discs in this way, you can expect degeneration, loss of disc height, and potential impingement of the corresponding spinal nerves.


When the cylindrical shape of the upper lumbar discs is not respected (left), or the wedge shape of the L5-S1 disc is not respected, there is compression, disc degeneration, and eventually pain and dysfunction.
With a return to correct anteversion of the pelvis (and a well-stacked spine), the cylindrical lumbar discs fit cleanly between the cylindrical vertebrae, and the wedge-shaped L5-S1 disc is given its own wedge-shaped space to call home. In this arrangement, the intervertebral discs can properly perform their shock absorber function while maintaining plenty of room for the segmental nerves to exit without compromise.

Well aligned vertebrae allow the spinal discs to perform their shock-absorbing function without compromise.
If you suffer from the variant of “forward pelvis” that includes problematic positioning of higher lumbar vertebrae, this can be caused by several things, each of which requires a different solution. If you are tensing the erector spine muscles (thrusting the buttocks backward or the chest forward), then the solution is to implement techniques to relax those muscles. Massage, stretching, and roller work are all good options. If the problem is a lack of tone in the abdominal wall, then you’ll want to seek out exercises to engage and strengthen the appropriate abdominal muscles.
It benefits pretty much everyone to find a healthy and natural curve at L5/S1 by sitting on a wedge to help tip the pelvis—and only the pelvis—forward, removing any counterproductive muscle tension. We have more detailed descriptions of how to properly “seat” your pelvis between your legs in our book, 8 Steps to a Pain Free Back.

It benefits almost everybody to use a wedge to help tip the pelvis - and only the pelvis - forward. This allows the vertebrae above to stack well without unhealthy muscle tension.
The lumbo-pelvic-hip-complex is made up of 15 bones and 29 muscles. With this many moving parts and a general lack of understanding about ideal human form, it’s no wonder that confusing and contradictory information abounds. Our aim is to shepherd you beyond non-specific descriptions of the pelvic area, and guide you towards healthy pelvic anteversion. This can go a long way toward resolving any low back pain and discomfort you have.
Join us in an upcoming Free Workshop (online or in person).
Find a Foundations Course in your area to get the full training on the Gokhale Method!
We also offer in person or online Initial Consultations with any of our qualified Gokhale Method teachers.




Comments
First thank you so, so much
Saddle stools are a big
Saddle stools are a big improvement on most chairs. I like them for short periods of sitting. Like you point out, they support pelvic anteversion and external leg rotation, which is huge. The challenges with saddle stools are:
I do recommend changing position frequently - my preference is stretchsitting (who can't use some extra stretch in their spine?), stacksitting (on a slope tailored to your pevlis), standing, samba, walking around, exercising, lying down. No chair does all that for you - it's you that needs to get up and move around - but I do like my chair to stretchsit and stacksit me.
This is a very interesting
"Crunches" are well-named -
"Crunches" are well-named - they crunch your discs and your spinal nerves! Situps have been weeded out of the Canadian Armed Forces regimen. My prediction is that crunches will be next for similar reasons. Here's a discussion of the subject: http://blog.bonati.com/us-army-phasing-out-sit-ups-due-to-spine-injuries/
Where is the evidence for the
Add New Comment
Login to add commment
Login