The #1 Reason Parents Get Back Pain
Women’s Empowerment Through Posture
My Three Favorite Posture Podcasts
Fixing Plantar Fasciitis
Function over Appearance: MommaStrong, the Gokhale Method, and Posture for Moms
Posture and pregnancy have always been closely linked for me. As you may know, my own journey to create the Gokhale Method and a life free of back pain began with my development of crippling back pain during pregnancy. So it’s always a special gift to get to connect with other mothers who understand the deep relationship between posture and health, and to help other women learn to navigate the many changes that come with pregnancy and childbirth.
That’s why I’ve teamed up with MommaStrong to bring you this discussion between me and Courtney Wyckoff, the founder of MommaStrong. She’s a Certified Personal Trainer and Corrective Exercise Specialist, with 16 years experience in the field of
Posture and Pregnancy: A Report
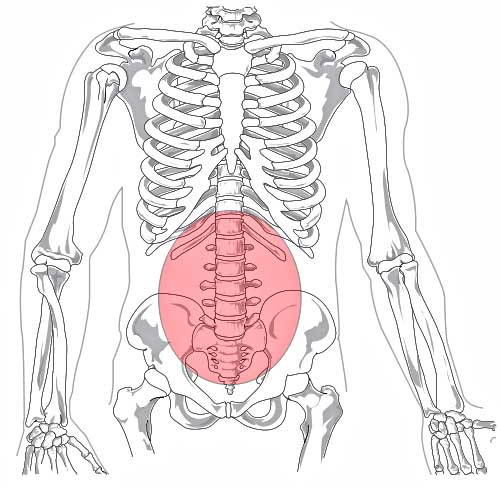
During my first pregnancy in 2011–12 I had — compared with other women — only a little trouble; I felt relatively fit. At the time, the occasional pain in my lower back and my permanent shoulder/ neck pain seemed normal because I had suffered them since I was in school. This fit with my modern comprehension of being healthy. Some aches and pains are not unusual. Upright posture? So not cool...
Here’s how I used to sit some years before my first pregnancy. I already suffered from occasional pain in my lower back and from permanent shoulder/ neck pain.
At the end of my pregnancy, my lower back pain became stronger. I started to suffer from sciatic nerve pain, which eventually covered the whole