Ex Your Back Pain, Use Your X-ray Eyes
Tom Carter’s Back Pain Success Story
Kathy Nauman Success Story
Sheila Bond’s Back Pain Journey
How Not To Do Yoga
"I Know What It's Like to Lose Hope:" Anissa's Posture Journey
Anissa Morgan is 46 years old and was born and raised in San Antonio, Texas. In her own words, her relationship with her body has “always been a little messed up.” She didn’t like how she looked. Growing up, her mom frequently told her that she was slouching and "should pull her shoulders back," anecdotal posture advice many of us have heard.
In adulthood, Anissa spent some time in the Army Reserves as a petroleum specialist. The military approach to posture reinforced what she’d heard from her mom in childhood: that she “shouldn’t be slouching and that everything should look ‘a certain way.’” In her job, she would deliver fuel to military vehicles such as airplanes, cars, and trucks. She
Abigayil Tamara's Experience with the Gokhale Method
We set a high bar for our six-lesson Gokhale Method Foundations course. We expect our students will
Sit, stand, walk, lie, and bend in new (old!) and better waysExperience significantly less pain and more functionExpect more from their body and life. Use the word “life-transforming” somewhere in their evaluation forms.Even with this high bar, a student sometimes surprises us with the extent or speed of their progress over the course. Abigayil Tamara is one such student - here is her story.
My Experience With the Gokhale Method
~Abigayil Tamara, MA, MSW
I looked into the Gokhale Method after someone in a grocery store told me how much it had helped his mother.
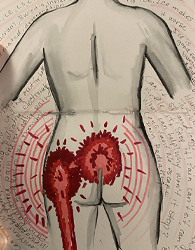
My back issues began over 34 years