How to Improve the Outcome of Spine Surgery (When It’s Needed)
Spinal surgery has come under a lot of flak in recent years for being an expensive and invasive treatment for back pain that yields poor results. Not many people see improvement in their pain a year after surgery, and many are worse off. Recovery from surgery can be also be very difficult.
Surgery should indeed be a last resort for most kinds of back pain. But sometimes surgery is needed to treat damage to spinal nerves, discs, or surrounding tissues, and we are very fortunate that there are people who have gone to school for years / decades and honed the necessary skills to right some wrongs in our bodies. The question then becomes, what can we do around the surgery to support the handiwork of the surgeon? To answer that question, it helps to understand some of the problems facing surgical patients post-surgery:
After surgery and during recovery, people tend to return to the same old practices which got them into trouble in the first place. Most people (and their doctors) don’t realize the critical role posture plays in causing the problems that led to surgery, and continues to play post-surgery. Surgery seems to get put in an exalted place where something as pedestrian as posture couldn’t possibly be relevant. Even if patients and/or doctors realize there’s a posture problem in the equation, they don’t know how to fix it (“sit up straight” is not the answer!). So once out of surgery, patients go back to the same round-backed bending or tucked tail sitting that caused the herniated disc or pinched nerve the surgeon just fixed. With an involved surgery like a spinal fusion, the stresses placed upon the spine from poor posture simply transfer to the next weakest area, usually just above or below the fusion, and the person is at risk of experiencing pain and dysfunction all over again.

When someone goes back to a lifestyle of excessive rounding or swaying after surgery, the risk of being in pain again is high. Photo courtesy Unsplash (rawpixel).
Some existing post-surgical therapies are rough, and can undo the delicate work of the surgeons. When I presented a Grand Rounds for the neurosurgery department at Stanford, I asked to sit in on a Grand Round as part of my preparation. This was interesting in many ways, including that it allowed me to overhear some informal conversation among the surgeons ahead of the talk. I heard a couple of surgeons talk about how they don’t refer their patients to any follow up therapy because they had seen too many patients handled roughly, encouraged to “push through pain,” and such. Some types of treatments for back pain routinely manipulate spinal joints beyond their normal range of motion. This can cause stress and trauma to joints, bones, and other tissues, especially in a post-surgical spine.
Recovery from surgery often includes a period of immobility, reduced activity, and unusual positioning, each of which are stressful in themselves. Prehab is not often recognized as necessary, desirable, or even relevant. Patients therefore often go into surgery in a particularly weakened and vulnerable condition, which can negatively affect the chances of success.

Often, recovery from a surgery is strenuous and causes some of the surgery’s progress to be undone. Photo courtesy Unsplash (rawpixel).
My recommendations to anyone considering or facing surgery are:
Understand the root of your problem. This would ideally include understanding why the problem happened, why it won’t heal on its own, and the relationship between your posture and the condition of your spine. The Gokhale Method provides this understanding intellectually, visually, and kinesthetically. It makes sense, looks right, and feels right. At best, you will give yourself a chance to avoid surgery. If you do need surgery, you will understand how not to recreate your problem. I speak from personal experience gotten the hard way. After having surgery to address a herniated L5-S1 disc, I reherniated the same disc a year later. I had no idea why at the time. With my acquired understanding, I not only avoided repeating the problem in my spinal discs, but also managed to heal the reherniation without going through a second (recommended) surgery.
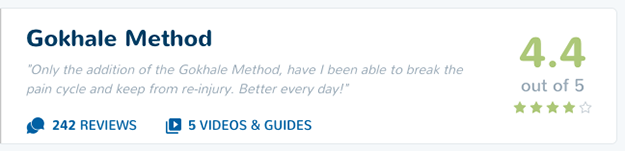
Explore all conservative measures first. Most interventions don’t result in a non-reversible change in your body. If they don’t work, there’s no harm done (except perhaps to your morale and a little to your pocketbook), and you move on. Surgery is non-reversible. So unless it’s extremely clearly indicated, it should be a last resort. A good resource for checking into how effective the many available back pain interventions are is healthoutcome.org, a crowdsourcing website that has gathered 1000s of ratings on 44 back pain interventions. The Gokhale Method is the top-rated of all of these with a 4.4 out of 5 rating and nearly 250 ratings (as of Nov. 27, 2018).
Optimize your prehab and rehab. The Gokhale Method teaches you how to sit, stand, lie, bend, and walk in ways that
won’t stress your spinal tissues (this is important post-surgery). This includes learning healthy alternate sleeping and sitting positions, since your habitual ones may not be possible because of the location of the incision.
strengthen your muscles, rehydrate your spinal discs, and otherwise prepare you for the challenges that necessarily accompany surgery. Sometimes people have the notion that Gokhale Method training is best put off until after surgery. This is unfortunate because the techniques can help improve the outcome from surgery.
Have you had back surgery? What has been your experience? Did you use the Gokhale Method for prehab or rehab?

Comments
I had a microdiscectomy on
I had a microdiscectomy on the L5 S1 about 5 years ago. The reason I chose surgery was because I had shooting pains in my leg and back that mostly happened at night. For months I tried alternative methods to eleviate the pain - exercise, physical therapy, accupuncture, etc., but nothing worked. At the time, hydrocodone was prescribed more regularly by doctors, and I was waking up every 2 hours with shooting pains and would have to take more hydrocodone just to sleep. It hurt just to lie down - a shooting, stabbing pain. Luckily, I only had to take pain drugs at night. After 3-4 months of this, I finally I cried uncle and signed up for surgery. Oh, how I wish I had never done that - and that I'd discovered the Gokhale method instead. I'm convinced that if I had, I might not have needed surgery.
Something must have gone wrong during surgery because I have somehow ended up with permanent nerve damage. Soon after surgery, I started getting numbness in my right toes. I called the surgeon and he ordered a MRI. No evidence of damage showed up. But the numbness and pain gradually over the months and years has increased and moved up my leg to the front of my thigh and even to some nerves between my legs. The first year, I went to multiple doctors and had multiple MRI's and all showed no damage. But the pain remains and has only increased. It is worse at night, luckily, but sometimes it wakes me up at night. It's not the shooting pain I had before, but more a dull intense ache. Almost every single day and night for the past 5 years, I have regretted the surgery. I am convinced that the surgery must have permanently damaged nerves.
In the meantime, I have read and re-read Gokhale's book, 8 Steps to a Pain-Free Back, and I believe that practicing her methods has helped me not injure my back further. As a very tall women, I was prone to slumping, and I sat at a desk many hours a day for my job. Now I walk with good posture and have vastly strengthened my core muscles, simply by walking and being aware of correct posture that Gokhale teaches. And any person who mentions back pain to me or even an interest in surgery, I tell them my story and beg them to read the book and practice her methods before going under the knife.
We're trying very hard to
We're trying very hard to reach as many people as we can - and you're helping!
I'm glad the book is helping you improve your posture and not injure your back further. I suspect more benefits are possible, but likely need more customized coaching. Try reaching out to one of our teachers for a session, preferably in-person so you can get hands-on help, but if that's not possible, over Skype / Zoom.
Wishing you on-going improvements - don't give up!
I have had scoliosis since
I have had scoliosis since birth (I am 79) but never problematic till this year.(my husband died 3 years ago and I sudenlly had many different health problems.) I am a body oriented person, worked with your book for a year (and gave copies to all of my children). One morning 7 months woke up with numbness in thigh and increasingly bad limp.
7 months later I had minimally invasive surgery recommended by two neurosurgeons, based on MRI: foraminotomy, laminectomy, spinal fusion - 2 small titanium rods to limit the scoliosis progressing.
I prepped by several sessions with a neurological physical therapist in the two months before surgery, took weekly class in strength and balance in the previous 6 months, did tai chi chi 3 times a week in the previous 6 months.
Surgery was successful: I am taller (see from higher now), stack the parts of my body more effertlessly and more symmetrically, walk without limping (especially when I remember to engage core mussels.
Two weeks post op I began to have severe pain in the femoral nerve which surgeon attributed to old blood left over from the surgery causing inflamation in around the nerve. Prescripbed Methyprednisonolendospak and Gabapentin. Effective immediately.
I have just sent for back back support for my desk chair.
Now the post op pain is gone, I am a very "happy camper" again.
All very great information
All very great information and I am going to pass this blog post on to one of my clients going in for back surgery this week. Your technique is amazing and works!!!
I loved this article Esther;
I loved this article Esther; since I am a had a fusion 4 years ago with excellent results. My only add would be:
The typical post op spine precautions are no BLT -- No Bending, Lifting and Twisting. The Gokhale Method teaches each of these things; using the hip hinge, lifting with the Inner Corset and no twisting postures. Yay!
I teach the Method to keep my spine hygiene in check.
amy
Add New Comment
Login to add commment
Login