How to Fix a Tight Psoas
When students first meet with a Gokhale Method® teacher they are sometimes surprised to learn that one of the reasons for their back pain is a tight psoas muscle. What does this little-known muscle, embedded deep within our bodies, have to do with back pain? And what do we need to do to have it recede in the background and leave our backs alone?
Get to know your psoas muscle
Psoas major (pronounced so-as) is a deep-lying muscle with a downwards trajectory through the abdomen. There can be some individual variation, but it usually originates from T12-L4, and it inserts at the lesser trochanter of the femur. Its main job is to contract and pull the thigh up—as in walking, running, and climbing, for example.
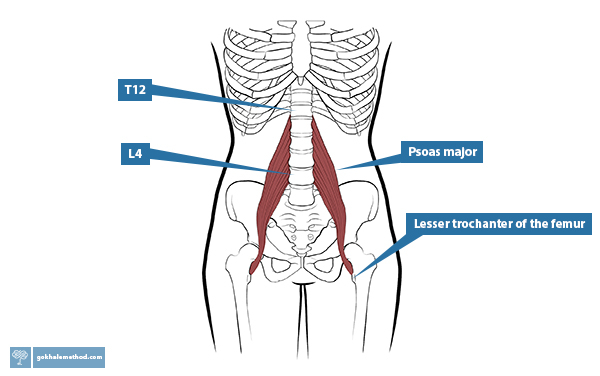
The psoas muscle lifts your thigh—or pulls on your lower back, depending on how it’s used.
For those who are not offended by meat analogies, this muscle is the filet mignon, or the tenderloin—it is meant to be lean, juicy, malleable, and stretchy. But in modern industrial populations, the psoas is often somewhat dry, tough, and short. The shortened length and tightness of the muscle can wreak havoc on the spine as it pulls forward on the lumbar spine, causing compression, wear and tear, and pain.
How do I know if I have a tight psoas?
There are various signs and symptoms associated with a tight psoas, including:
- A pronounced sway in the lumbar area
- Pain when going from sitting to standing
- Back pain either caused or eased by walking
- A sore insertion point on the thigh
- Feeling stiff and unable to straighten up, or “vulnerable” in the lower back, especially first thing in the morning
Why did my psoas get tight?
- Sitting for extended periods without movement breaks is one reason that our psoas adapts to a shorter length because the muscle then spends a long time at the shorter end of the range of what it can do.
- The shortening effect of sitting is made more likely when we sit poorly with our pelvis tucked. A modern issue with sitting is that we have poorly designed furniture, such as bucket seats and deep sofas, which encourage us to tuck and slouch.

Most modern furniture is designed for aesthetic appeal rather than to enable us to sit well. Image from: Pexels
- Back pain patients are often recommended to use a chair with built in lumbar support, or to add a lumbar cushion. The extra curvature then reinforces a habit of swaying the lower back, which in turn enables the psoas to remain short and tight.
Most backrests follow the S-shaped spine paradigm and are designed to give “lumbar support.” This creates exaggerated curvature and compression in the lumbar spine. (Google, n.d.)
- A tight psoas can also have a psychosomatic cause, as this muscle is deeply linked to both chronic stress and trauma responses in the body. We see this response even in babies in the Moro or startle reflex.
Restoring length in your psoas
A common remedy for a tight psoas is a lunge or other psoas stretch. Though effective, the problem with this approach is that it is not possible to do enough stretching to make a sustainable difference to the length of this muscle. The stretch feels good, but the muscle quickly goes back to its short resting length. For some people, if they have been stretching aggressively and the attachments of the muscle are inflamed, stretching can cause additional pain and dysfunction.
Another common approach is to get a gifted practitioner to “release” your psoas. This very intense maneuver can also be effective, but has the same problem as the stretching approach—it provides temporary relief, but does not sustainably reset the resting length of the muscle when poor daily posture is shortening it.
The only sustainable way I know of resetting a tight psoas is to recruit Nature’s solution for keeping this muscle healthy, which is to learn how to walk naturally/skillfully/effectively.
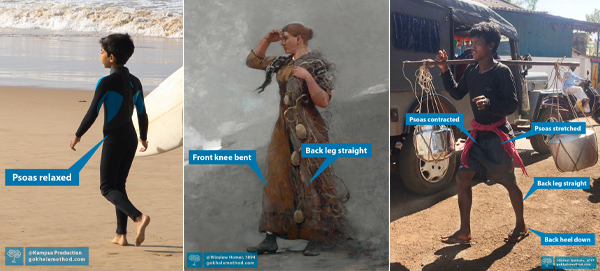
Our natural gait pattern is evident in our young children, our ancestors, and villagers in non-industrialized parts of the world. It gives the psoas muscle both the engagement and stretch it needs in a gentle and consistent way.
(central painting: Fisher Girl, Winslow Homer, 1894. Museum at Amherst College, Petegorsky/Gipe.)
Nature’s built-in solution to stretching your psoas
To describe the action of healthy walking, we use the term glidewalking. With this pattern, every step becomes a psoas stretch. Refinements in walking like learning to contract your glutes with every step and leaving your rear heel down for an extended time, augment the psoas stretch. If, however, you don’t know how to maintain a long, stable lumbar spine, these same improvements in gait can be counterproductive and pull your spine into additional sway.
![]()
Our PostureTracker™ wearable enables you to monitor and maintain your rib anchor and a healthy, stable spine as you walk (shown in green), naturally stretching your psoas. Here I am on the Alumni Live Chat in December last year, demonstrating.
![]()
PostureTracker™ will tell you (shown in red) if you forget your healthy posture cues! Notice that I have let my back sway severely at the end of my stride.
Advanced Glidewalking Course for Alumni
If you are an alumnus, you are encouraged to join me in our Advanced Glidewalking Course. This course is a comprehensive deep-dive to both revisit the basics of healthy, natural walking, refine its many components, and learn advanced techniques that are not included in our beginner courses. Your psoas will thank you! Six weekly lessons start Wednesday, February 28, 11 a.m. (PST), 8 p.m. (CET). You can sign up here.
Best next action steps for newcomers
If you are new to the Gokhale Method, get started by booking a consultation, online, or in person with one of our teachers to find out how the Gokhale Method can help you.
You can sign up below to join any one of our upcoming FREE Online Workshops. . .

Comments
I think addressing a tight…
Hello @ fall guys, I think addressing a tight psoas requires a multifaceted approach:
Add New Comment
Login to add commment
Login